pulmonary adenocarcinoma
Image Gallery
[ ( ||image_reduire{0,60}|inserer_attribut{alt,Pulmonary adenocarcinoma})
]
||image_reduire{0,60}|inserer_attribut{alt,Pulmonary adenocarcinoma})
]
Adenocarcinoma is the most common type of lung cancer in contemporary series, accounting for approximately one-half of lung cancer cases (about 50%).
The increased incidence of adenocarcinoma is thought to be due to the introduction of low-tar filter cigarettes in the 1960s, although such causality is unproven.
Microscopy
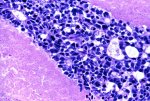
Histologic diagnosis requires evidence of either neoplastic gland formation or intracytoplasmic mucin.
There is significant variation in the extent and architecture of neoplastic gland formation, ranging from well-formed acini to more papillary and even cribriform types.
The solid type of adenocarcinoma lacks the architectural characteristics of better differentiated tumors and is indistinguishable from large cell undifferentiated carcinoma except for the presence of intracellular mucin.
The detection of intracellular mucin requires special histochemical stains, such as mucicarmine or Periodic Acid-Schiff (PAS)
![]() malignant glandular structures with central lumina
malignant glandular structures with central lumina
![]() some of which contain intraluminal mucinous-like material.
some of which contain intraluminal mucinous-like material.
![]() extensive areas of necrosis
extensive areas of necrosis
2011 IASLC/ATS/ERS classification of adenocarcinoma
The 2011 schema from the IASLC/ATS/ERS incorporates a number of changes in the classification of patients with adenocarcinoma:
The term "bronchioloalveolar carcinoma" (BAC) is eliminated. Lesions that were formerly classified as BAC are now placed in one of several categories that appear to correlate with the stages of transformation into widely invasive adenocarcinoma. The early stages of these lesions include the following:
![]() Atypical adenomatous hyperplasia (AAH), an entity that was previously recognized in the WHO system as a preinvasive lesion for lung adenocarcinoma.
Atypical adenomatous hyperplasia (AAH), an entity that was previously recognized in the WHO system as a preinvasive lesion for lung adenocarcinoma.
![]() Adenocarcinoma in situ (AIS) is a localized (≤3 cm) adenocarcinoma in which growth is restricted to tumor cells growing along alveolar structures (lepidic growth pattern) and lacks any component of invasion. Most AIS tumors are nonmucinous. Mucinous lesions comprise a small subset of such tumors. Observational studies indicate that AIS has a 100 percent cancer-specific survival if completely resected. AIS was previously categorized as bronchioloalveolar carcinoma in the 2004 WHO system.
Adenocarcinoma in situ (AIS) is a localized (≤3 cm) adenocarcinoma in which growth is restricted to tumor cells growing along alveolar structures (lepidic growth pattern) and lacks any component of invasion. Most AIS tumors are nonmucinous. Mucinous lesions comprise a small subset of such tumors. Observational studies indicate that AIS has a 100 percent cancer-specific survival if completely resected. AIS was previously categorized as bronchioloalveolar carcinoma in the 2004 WHO system.
![]() Minimally invasive adenocarcinoma is a small, solitary adenocarcinoma (≤3 cm) with a predominantly lepidic growth pattern and less than or equal to 5 mm invasion. Most but not all of these lesions are nonmucinous. The cancer-free survival in these patients should approach 100 percent with complete surgical resection, based upon observational studies.
Minimally invasive adenocarcinoma is a small, solitary adenocarcinoma (≤3 cm) with a predominantly lepidic growth pattern and less than or equal to 5 mm invasion. Most but not all of these lesions are nonmucinous. The cancer-free survival in these patients should approach 100 percent with complete surgical resection, based upon observational studies.
![]() Invasive adenocarcinomas are classified by their predominant pattern. As an example, invasive non-mucinous bronchioloalveolar lesions are classified as invasive adenocarcinoma, lepidic predominant. Other patterns include acinar, papillary, micropapillary, and solid predominant with mucin production.
Invasive adenocarcinomas are classified by their predominant pattern. As an example, invasive non-mucinous bronchioloalveolar lesions are classified as invasive adenocarcinoma, lepidic predominant. Other patterns include acinar, papillary, micropapillary, and solid predominant with mucin production.
![]() Invasive mucinous adenocarcinoma (formerly mucinous bronchioloalveolar pattern) is now classified as a separate variant, the implication being that most of what was formerly called mucinous BAC represented invasive adenocarcinomas.
Invasive mucinous adenocarcinoma (formerly mucinous bronchioloalveolar pattern) is now classified as a separate variant, the implication being that most of what was formerly called mucinous BAC represented invasive adenocarcinomas.
![]() Other variants of invasive adenocarcinoma include colloid, fetal, and enteric adenocarcinoma.
Other variants of invasive adenocarcinoma include colloid, fetal, and enteric adenocarcinoma.
![]() For lesions without identifiable adenocarcinoma patterns present but in which immunohistochemical stains support the diagnosis of adenocarcinoma, the terminology “Non-small cell carcinoma, favor adenocarcinoma” is used.
For lesions without identifiable adenocarcinoma patterns present but in which immunohistochemical stains support the diagnosis of adenocarcinoma, the terminology “Non-small cell carcinoma, favor adenocarcinoma” is used.
2011 IASLC classification
The 2011 IASLC/ATS/ERS schema stresses the radiographic correlates of this approach to classification. Examples of this approach include the following:
![]() The preinvasive AAH and non-mucinous AIS characteristically have a ground glass radiographic appearance. Minimally invasive non-mucinous lesions may have a predominantly ground glass appearance with a smaller solid component.
The preinvasive AAH and non-mucinous AIS characteristically have a ground glass radiographic appearance. Minimally invasive non-mucinous lesions may have a predominantly ground glass appearance with a smaller solid component.
![]() In contrast, mucinous AIS has a solid appearance on imaging.
In contrast, mucinous AIS has a solid appearance on imaging.
![]() The radiographic and molecular correlations of the different subtypes are shown in the attached table.
The radiographic and molecular correlations of the different subtypes are shown in the attached table.
The 2011 IASLC/ATS/ERS document also emphasizes that tissue specimens should be managed not only for pathologic diagnosis, but to preserve tissue for molecular studies.
For patients with advanced lung adenocarcinoma, tissue should be tested for the presence of epidermal growth factor receptor (EGFR) mutation status as well as potentially for other molecular abnormalities that could affect subsequent therapy.
Types (2004 WHO classification of adenocarcinoma)
In the 2004 World Health Organization schema, adenocarcinoma is divided into a number of subtypes. Although it remains to be seen whether the WHO adopts the new classification scheme for adenocarcinoma, the 2004 classification defined some entities more specifically, and introduced some new entities, most of which are retained in the new proposed classification.
![]() pulmonary acinar adenocarcinoma
pulmonary acinar adenocarcinoma
![]() pulmonary papillary adenocarcinoma
pulmonary papillary adenocarcinoma
![]() pulmonary bronchioloalveolar adenocarcinoma
pulmonary bronchioloalveolar adenocarcinoma
![]() pulmonary solid adenocarcinoma
pulmonary solid adenocarcinoma
![]() pulmonary clear cell adenocarcinoma
pulmonary clear cell adenocarcinoma
![]() pulmonary mucinous adenocarcinoma (colloid)
pulmonary mucinous adenocarcinoma (colloid)
![]() pulmonary mucinous cystadenocarcinoma
pulmonary mucinous cystadenocarcinoma
![]() pulmonary signet ring adenocarcinoma
pulmonary signet ring adenocarcinoma
![]() pulmonary mixed adenocarcinoma
pulmonary mixed adenocarcinoma
![]() pulmonary fetal adenocarcinoma
pulmonary fetal adenocarcinoma
- low-grade adenocarcinoma of fetal lung type (L-FLAC)
- high-grade adenocarcinoma of fetal lung type (H-FLAC)
Grading systems : #20551825#
Variants
![]() pulmonary adenocarcinomas with enteric differentiation (#15832091#)
pulmonary adenocarcinomas with enteric differentiation (#15832091#)
Comparative genomic hybridization (CGH)
CGH revealed regions on 1q, 2p, 3q, 5p, 5q, 7p, 8q, 11q, 12q, 14q, 16p, 17p, 19q, 20q, 21q, and 22q to be commonly overrepresented and regions on 2q, 3p, 4p, 5q, 7q, 8p, 9p, 13q, 14q, and 17p to be underrepresented.
![]() 16p13 gain (50%)
16p13 gain (50%)
- 16p13 amplification was associated with relatively poor differentiation and late stage.
Videos
![]() Pulmonary adenocarcinoma by Washington Deceit
Pulmonary adenocarcinoma by Washington Deceit
References
![]() A grading system of lung adenocarcinomas based on histologic pattern is predictive of disease recurrence in stage I tumors. Sica G, Yoshizawa A, Sima CS, Azzoli CG, Downey RJ, Rusch VW, Travis WD, Moreira AL. Am J Surg Pathol. 2010 Aug;34(8):1155-62. PMID: #20551825#
A grading system of lung adenocarcinomas based on histologic pattern is predictive of disease recurrence in stage I tumors. Sica G, Yoshizawa A, Sima CS, Azzoli CG, Downey RJ, Rusch VW, Travis WD, Moreira AL. Am J Surg Pathol. 2010 Aug;34(8):1155-62. PMID: #20551825#
![]() Shen H, Zhu Y, Wu YJ, Qiu HR, Shu YQ. Genomic alterations in lung adenocarcinomas detected by multicolor fluorescence in situ hybridization and comparative genomic hybridization. Cancer Genet Cytogenet. 2008 Mar;181(2):100-7. PMID: #18295661#
Shen H, Zhu Y, Wu YJ, Qiu HR, Shu YQ. Genomic alterations in lung adenocarcinomas detected by multicolor fluorescence in situ hybridization and comparative genomic hybridization. Cancer Genet Cytogenet. 2008 Mar;181(2):100-7. PMID: #18295661#
![]() Shibata T, Uryu S, Kokubu A, Hosoda F, Ohki M, Sakiyama T, Matsuno Y, Tsuchiya R, Kanai Y, Kondo T, Imoto I, Inazawa J, Hirohashi S. Genetic classification of lung adenocarcinoma based on array-based comparative genomic hybridization analysis: its association with clinicopathologic features. Clin Cancer Res. 2005 Sep 1;11(17):6177-85. PMID: #16144918#
Shibata T, Uryu S, Kokubu A, Hosoda F, Ohki M, Sakiyama T, Matsuno Y, Tsuchiya R, Kanai Y, Kondo T, Imoto I, Inazawa J, Hirohashi S. Genetic classification of lung adenocarcinoma based on array-based comparative genomic hybridization analysis: its association with clinicopathologic features. Clin Cancer Res. 2005 Sep 1;11(17):6177-85. PMID: #16144918#